ARE YOU GETTING ENOUGH SLEEP?
by Dr Alice McNamara
MOST OF US WOULD SAY “NO, I WOULD LOVE MORE SLEEP!” AND WE ARE LIKELY CORRECT!
Sleep is being described as the “Third Pillar of Health” next to the widely studied and spruiked pillars of Diet and Exercise. But really, this undersells sleep. Sleep is the foundation on which quality diet and exercise choices are made. With poor sleep, we have poor health. Sleep is the fundamental phase that our body repairs cells and DNA in muscles and brain tissue. It is where memories are consolidated, stress hormones regulated, immune system supercharged up and energy stores replenished and reserved.
In humans, complete sleep deprivation has been used as a means of interrogation, which has resulted in court trials over whether or not the technique is a form of torture. There are severe neurological and visual consequences of trying to avoid sleep altogether. The longest documented record of staying awake was set in 1965 by American high school student, Randy Gardner who abstained from sleep for 11 days and 25mins! But sleep deprivation known to be so bad for you, that the Guinness Book of Records has stopped publishing data as to deter further attempts. Laboratory rats deprived of sleep die within a matter of weeks and demonstrate impaired thermoregulatory and metabolic properties, meaning they get chronically overheated, and put on weight.
Most of us sit at a less extreme end of the spectrum, but also know we could do with more sleep.
Even this chronic, long-term, limited or poor sleep has long-term health consequences. Shift work is now listed by the World Health Organisation as a known carcinogen. Studies have found that “day sleep” doesn’t result in the same melatonin levels due to the brain’s response to light. Hence, there is a limited effect of “day sleep” on the flow-on hormonal levels and in actually repairing DNA. Over time, lack of night sleep and adequate melatonin release is likely to increase the risk of multiple cancers.
Over the next few months in this blog, we’ll work our way through some topics around the benefits of sleep for health, in pregnancy, in illness and injury states, across shift work, and in different periods of life.
SLEEP DEPRIVATION AND ITS CONSEQUENCES!
These are many and varied:
- Irritability
- Cognitive impairment
- Memory lapses or loss
- Impaired moral judgement
- Severe yawning
- Hallucinations
- Symptoms similar to ADHD in kids and adolescents
- Impaired immune system
- Risk of Type 2 Diabetes Mellitus
- Risk of Heart Disease
- Decreased reaction time and accuracy
- Tremors
- Aches
- Altered temperature regulation
- Growth suppression
- Risk of obesity
So, at what point do you perform like your blood alcohol is over 0.05?
- Remaining awake for 18-24 hours
- Having only 5 hours sleep for 4-5 nights
- In moderate to severe Obstructive Sleep Apnoea
If this is YOU, it may be best to avoid sending late-night work emails!
SO – ARE YOU GETTING ENOUGH SLEEP?
Sleep problems are very common. In 2011, Deloitte Access Economics described sleep disorders as a large and under-recognised problem in Australia*. In 2010 there were an estimated 1.5 million Australians (8.9% of the population) suffering from the three most common sleep disorders comprising approximately:
- 775,000 people with Obstructive Sleep Apnoea (OSA) (4.7%);
- 492,000 people with primary insomnia (3%); and
- 199,000 people with Restless Leg Syndrome (RLS) (1.2%)
Additionally, they anticipated that numbers would be underestimated, given many more people experience symptoms of insomnia, RLS or OSA than those who are formally diagnosed.
They calculated the total cost associated with sleep disorders at $36.4 billion ($27.0 billion to $42.8 billion) per year.
Loss of healthy life is measured in disability-adjusted life years (DALYs), and sleep deprivation does impact peoples quality of life. It was estimated 190,000 DALYs were lost due to sleep disorders in 2010. OSA contributed 109,000 DALYs, insomnia 56,000 DALYs and RLS 26,000 DALYs.
THE EPWORTH SLEEPINESS SCALE
We have been interested in analysing ourselves in relation to this question of “enough sleep” for many years now. Hospital sleep laboratories play in important role in diagnosing Obstructive Sleep Apnoea (OSA) through a method called Polysomnography, where a patient sleeps while their movements and oxygen levels are measured by sensors on the body overnight. We will talk more about OSA in a later blog.
“Do you get enough sleep” is generally a subjective question, and the tricky thing is that people get used to the impairment. With increasing days of sleep restriction there is an incremental decrease in your performance and increase in your daytime sleepiness. With increased sleep restriction you eventually see a plateau of symptoms. i.e. your objective performance is still bad but you get used to your experience of sleepiness!
In 1991 Murray Johns (from the Epworth Hospital in Melbourne) decided perception of a patients daytime sleepiness was likely to be a reliable measure of “enough sleep”. He tested this theory in his validation study in 1991 on 180 patients using a short questionnaire to measure how likely a person was to be excessively sleepy during the waking hours, indicating if they were deprived of good quality sleep. Today, the Epworth Sleepiness Scale s a widely used measure of daytime sleepiness with scores ranging from 0 to 24. Excessive daytime sleepiness is defined as a total score of ≥10.**
Answer it for yourself!
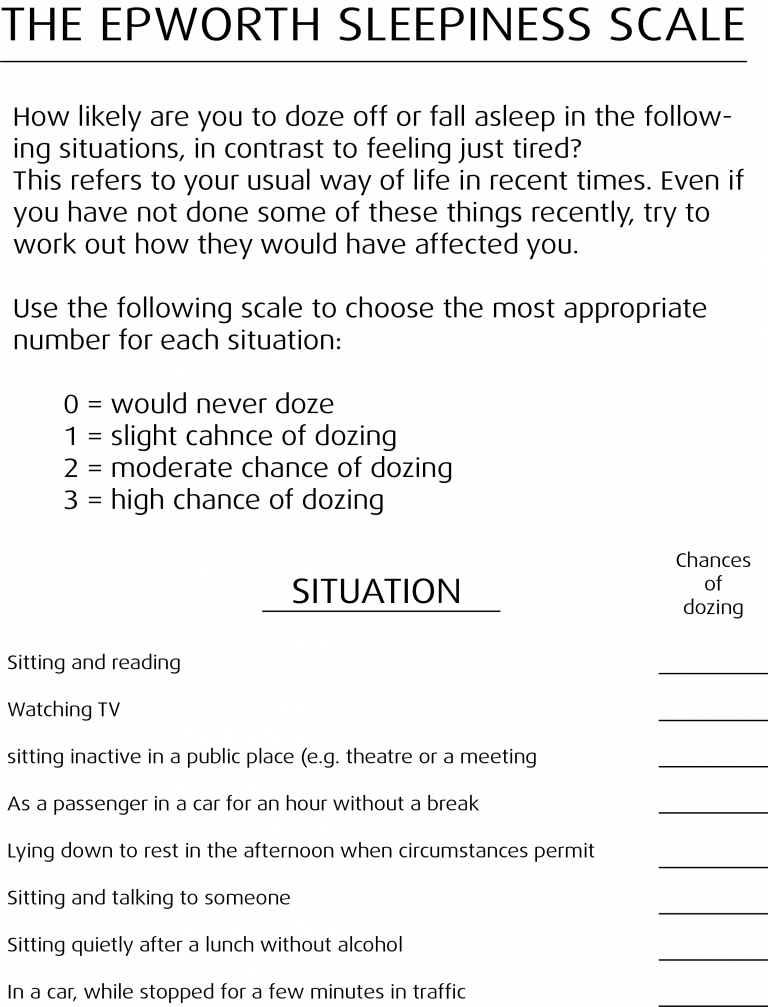
Where do you fit? In the original validation study published in 1991, the authors found that normal healthy people, mostly hospital workers with no diagnosed sleep problems (the controls), scored an average of 5.9. It’s designed that in healthy people, given the right circumstances like lying down in the afternoon, sleepiness is normal!
In contrast, primary snorers scored 6.5, people with Obstructive Sleep Apnoea 11.7, Restless Leg Syndrome 9.2, Narcolepsy 17.5, and Insomnia 2.2.
There is a longer questionnaire for those who are interested called the Pittsburgh Sleep Quality Index, which is worth a google if you are interested in further assessing your sleep quality.*** However, for most people (and it has been validated) the Epworth Sleepiness Scale gives a good assessment of where you are at.
WHAT ARE THE CAUSES OF DAYTIME SLEEPINESS?
Well, most commonly it is due to not enough quality sleep.
Lifestyle is the single most important reason that most people do not get enough sleep.
- Work hours, social engagements, commute time and recreational commitments
- Shift work
- Jet lag
- Sleep interruptions e.g. young children
But also medical sleep disorders are common, for which your GP can help:
- Sleep breathing disorders
- RLS/Periodic limb movement disorder
- Others
- Circadian disorders
- Drugs/alcohol/pain syndromes
- Neurological disease
- Insomnia, narcolepsy
- Idiopathic, hypersomnia, parasomnias
- Psychiatric disorders
SO WHAT CAN YOU DO?
The lifestyle factors are in your control. Careful scheduling to prioritise sleep, minimise commuting and eliminating some social events will free up more time for bed. There may be medical reasons your sleep is affected, and a visit to the GP for further tests and diagnoses may be helpful. Don’t expect that the answer to poor sleep is a sleeping tablet, as that solution is a bandaid to the real cause of the problem, and may lead to dependence on them. Likewise, alcohol is a sneaky devil. Don’t trust it. You may fall asleep, but your sleep quality and duration of the important sleep cycles is significantly impaired.
Commonly, anxiety around too little sleep or being unable to sleep will only fuel the problem.
Instead, be honest with yourself about how you can better prioritise sleep as your foundation pillar of health, invest in a quality bed and sleeping environment, and, definitely seek help if you need to.
zzz
*Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540–5.
**Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213.
***Deloitte Access Economics, as commissioned by the Sleep Health Foundation; Re-awakening Australia – The economic cost of sleep disorders in Australia, 2011. Accessed at https://www2.deloitte.com/au/en/pages/economics/articles/sleep-health.html# 24/02/18
Feel it for yourself
Find a TEMPUR store or Stockist and try out our range of mattresses for yourself

SIGN UP FOR THE NEWSLETTERS!
By signing up, you agree to receive TEMPUR Australia’s products, services, news, reviews and promotions by emails. For more information on how we process your personal data, please refer to our Privacy Policy.



